The exploration of stem cell therapy within regenerative medicine represents a significant stride toward addressing the complex challenge of degenerative disc disease (DDD), a prevalent cause of chronic low back pain. This debilitating condition, characterized by the deterioration of the intervertebral discs, serves as a primary contributor to the global burden of musculoskeletal disability. Traditional management strategies, while effective in symptom alleviation, fall short of addressing the underlying pathology, thereby necessitating the pursuit of innovative therapeutic approaches. The application of stem cell therapy in this domain embodies the confluence of scientific curiosity and clinical need, heralding a paradigm shift in the treatment of DDD.
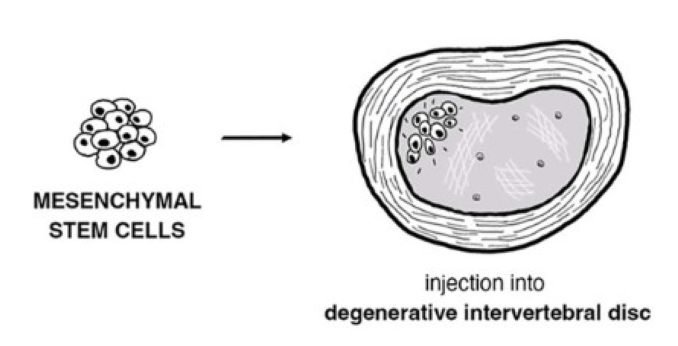
Degenerative disc disease emerges from the progressive loss of disc integrity, leading to diminished shock absorption and flexibility within the spinal column. The affliction is marked by a cascade of cellular and molecular deteriorations, culminating in chronic pain and functional impairment. Stem cell therapy, rooted in the principles of regenerative medicine, offers a promising avenue for halting or even reversing this degenerative process. By leveraging the pluripotent characteristics of stem cells, specifically mesenchymal stem cells (MSCs), this approach aims to rejuvenate the damaged disc matrix, restore disc height, and alleviate inflammation.
Preclinical Promise: Insights from Animal Models
Animal studies have been instrumental in elucidating the potential mechanisms through which stem cell therapy exerts its regenerative effects. The implantation of MSCs into degenerated discs of animal models has demonstrated encouraging outcomes, including the restoration of disc height, enhanced hydration, and a reduction in inflammatory markers. These findings not only underscore the feasibility of stem cell application in disc regeneration but also highlight the critical role of the cellular microenvironment in determining therapeutic success.
The translation of stem cell therapy from preclinical promise to clinical potential necessitates a meticulous evaluation of safety, efficacy, and mechanism of action. Early-phase clinical trials have reported promising results, such as significant pain reduction and indications of disc regeneration. However, the path to widespread clinical adoption is fraught with challenges. Key among these is the need to optimize the survival, integration, and differentiation of implanted stem cells within the harsh microenvironment of the degenerated disc. Furthermore, the heterogeneity of DDD pathology and patient-specific factors add layers of complexity to the therapeutic design.
The methodological underpinnings of stem cell therapy for DDD involve the isolation, expansion, and targeted implantation of MSCs into the affected disc space. Clinical trials to date have adopted varying protocols with respect to stem cell sourcing, preparation, and delivery methodologies, reflecting the nascent state of this therapeutic approach. Despite the variability, a consistent theme across studies is the observed improvement in patient-reported outcomes, including pain and functional status. Nonetheless, the absence of large-scale, randomized controlled trials and long-term follow-up data underscores the preliminary nature of these findings.
The discussion surrounding stem cell therapy for DDD is characterized by cautious optimism. While the therapeutic potential is evident, several dilemmas persist, including the precise mechanisms of stem cell-induced regeneration, the optimal cell type and delivery method, and the long-term safety and efficacy of the treatment. Addressing these issues requires a multidisciplinary effort, integrating insights from cellular biology, biomaterial science, and clinical orthopedics.
Stem cell therapy emerges as a frontier technology in the battle against degenerative disc disease, offering a glimpse into a future where the restoration of disc integrity and function is attainable. The journey from laboratory research to clinical application is marked by significant achievements and formidable challenges alike. As we advance, it is imperative that future research endeavors are guided by a commitment to rigorous scientific inquiry, ethical considerations, and patient-centric care. The realization of stem cell therapy’s full potential in treating DDD will not only represent a milestone in regenerative medicine but also a substantial leap forward in improving the quality of life for millions affected by chronic back pain.
The path forward necessitates a concerted effort to expand the body of evidence through well-designed clinical trials, enhance the understanding of stem cell biology in the context of disc regeneration, and refine therapeutic protocols to ensure the highest standards of safety and efficacy. By embracing these challenges, the medical community can unlock the transformative promise of stem cell therapy, transitioning from the realm of potential to a reality of clinical practice that redefines the management of degenerative disc disease.
The translation of the preceding English text in Slovenian:
Raziskovanje terapije z matičnimi celicami znotraj regenerativne medicine predstavlja pomemben korak naprej pri naslavljanju kompleksnega izziva degenerativne bolezni diskov (DDD), pogostega vzroka kronične bolečine v spodnjem delu hrbta. To onemogočajoče stanje, za katerega je značilno poslabšanje medvretenčnih diskov, predstavlja glavni prispevek k globalnemu bremenu mišično-skeletne invalidnosti. Tradicionalne strategije upravljanja, čeprav učinkovite pri lajšanju simptomov, ne naslavljajo osnovne patologije, kar zahteva iskanje inovativnih terapevtskih pristopov. Uporaba terapije z matičnimi celicami na tem področju uteleša sovpadanje znanstvene radovednosti in klinične potrebe, napovedujoč premik paradigme pri zdravljenju DDD.
Degenerativna bolezen diskov izhaja iz postopne izgube integritete diska, kar vodi v zmanjšano absorpcijo šoka in fleksibilnost znotraj hrbteničnega stolpca. Bolezen je zaznamovana z nizom celičnih in molekularnih poslabšanj, ki se končajo s kronično bolečino in funkcionalno okvaro. Terapija z matičnimi celicami, utemeljena na načelih regenerativne medicine, ponuja obetaven pristop za ustavitev ali celo obrnitev tega degenerativnega procesa. Z izkoriščanjem pluripotentnih lastnosti matičnih celic, posebej mezenhimskih matičnih celic (MSC), ta pristop cilja na pomlajevanje poškodovane diskovne matrike, obnovo višine diska in lajšanje vnetja.
Predklinična obljuba: Uvidi iz živalskih modelov
Živalske študije so bile ključne pri razjasnitvi potencialnih mehanizmov, preko katerih terapija z matičnimi celicami izvaja svoje regenerativne učinke. Implantacija MSC v degenerirane diske živalskih modelov je pokazala spodbudne rezultate, vključno z obnovo višine diska, izboljšano hidracijo in zmanjšanjem vnetnih označevalcev. Ti ugotovitve ne poudarjajo le izvedljivosti uporabe matičnih celic pri regeneraciji diskov, ampak tudi poudarjajo ključno vlogo celičnega mikrookolja pri določanju terapevtskega uspeha.
Prevod terapije z matičnimi celicami iz predklinične obljube v klinični potencial zahteva skrbno oceno varnosti, učinkovitosti in mehanizma delovanja. Zgodnje klinične študije so poročale o obetavnih rezultatih, kot so pomembno zmanjšanje bolečine in znaki regeneracije diska. Vendar pa je pot do široke klinične uporabe polna izzivov. Med temi je ključnega pomena potreba po optimizaciji preživetja, integracije in diferenciacije vsajenih matičnih celic znotraj ostrega mikrookolja degeneriranega diska. Poleg tega heterogenost patologije DDD in specifični dejavniki pacientov dodajajo plasti kompleksnosti terapevtskemu načrtovanju.
Metodološke osnove terapije z matičnimi celicami za DDD vključujejo izolacijo, razširitev in ciljano vsaditev MSC v prizadeti diskovni prost
or. Klinične študije do sedaj so sprejele različne protokole glede na vir matičnih celic, pripravo in načine dostave, kar odraža začetno stanje tega terapevtskega pristopa. Kljub raznolikosti je skupna tema med študijami opaženo izboljšanje v poročanih izidih pacientov, vključno z bolečino in funkcionalnim statusom. Kljub temu odsotnost obsežnih, naključno nadzorovanih preskušanj in dolgoročnih podatkov o spremljanju poudarja predhodno naravo teh ugotovitev.
Razprava o terapiji z matičnimi celicami za DDD je zaznamovana s previdnim optimizmom. Čeprav je terapevtski potencial očiten, ostaja več dilem, vključno z natančnimi mehanizmi regeneracije, ki jih povzročajo matične celice, optimalno vrsto celic in metodo dostave ter dolgoročno varnostjo in učinkovitostjo zdravljenja. Naslavljanje teh vprašanj zahteva multidisciplinarni napor, ki vključuje vpoglede iz celične biologije, znanosti o biomaterialih in klinične ortopedije.
Terapija z matičnimi celicami se pojavlja kot tehnologija meje v boju proti degenerativni bolezni diskov, ki ponuja vpogled v prihodnost, kjer je obnova integritete in funkcije diska dosegljiva. Pot od laboratorijskih raziskav do klinične uporabe je zaznamovana z znatnimi dosežki in formidabilnimi izzivi. Ko napredujemo, je nujno, da prihodnja raziskovalna prizadevanja vodijo zavezanost k rigoroznemu znanstvenemu poizvedovanju, etičnim premislekom in osredotočenostjo na pacienta. Uresničitev polnega potenciala terapije z matičnimi celicami pri zdravljenju DDD ne bo predstavljala le mejnika v regenerativni medicini, ampak tudi znaten korak naprej pri izboljšanju kakovosti življenja milijonov, prizadetih zaradi kronične bolečine v hrbtu.
Pot naprej zahteva usklajen napor za širitev telesa dokazov preko dobro zasnovanih kliničnih preskušanj, izboljšanje razumevanja biologije matičnih celic v kontekstu regeneracije diska in izpopolnitev terapevtskih protokolov za zagotavljanje najvišjih standardov varnosti in učinkovitosti. Z objemom teh izzivov lahko medicinska skupnost odklene preobrazbeno obljubo terapije z matičnimi celicami, prehajajoč iz sfere potenciala v realnost klinične prakse, ki preoblikuje upravljanje degenerativne bolezni diskov.
Reference: Munda M, Velnar T. Stem cell therapy for degenerative disc disease: Bridging the gap between preclinical promise and clinical potential. Biomol Biomed [Internet]. 2023 Sep. 4 [cited 2024 Feb. 11];. Available from: https://www.bjbms.org/ojs/index.php/bjbms/article/view/9518
Editor: Ermina Vukalic
Leave a Reply