Background
The incidence of out-of–hospital-cardiac-arrest (OHCA) in Europe is in average 84 cases/100.000 population /year with achieved return of spontaneous circulation (ROSC) in 9% – 50% of resuscitation attempt and survival to discharge of admitted patients in 6.4% – 66.9%. Majority of admitted OHCA patients are usually comatose, intubated and mechanically ventilated. Post-cardiac arrest brain injury is most widely assessed by Cerebral Performance Category (CPC) scale and corresponds to quality of life and outcome. CPC categories I and II represent good neurological outcome, severe brain injury includes CPC categories III-V.
Why Was This Study Done?
According to trials, most significant and well-known independent predictors of neurological dysfunction after OHCA are prehospital data such as asystole as the cause of OHCA, long resuscitation time in addition to the absence of corneal and pupillary reflexes, absence of motoric response on admission, adrenalin therapy, metabolic acidosis and admission arterial pCO2 <4,5 kPa. Our aim was to evaluate the relationship between clinical parameters of the post-resuscitation period and neurological outcome in OHCA patients, when all recommended therapeutic strategies, including hypothermia, were on board.
What Did the Researchers Do and Find?
The group of researchers from the University clinical center Maribor performed a retrospective observational study and included 110 patients, successfully resuscitated in the out-of-hospital settings and admitted alive to the Department of medical intensive care (MICU) of the tertiary University clinical center Maribor (Slovenia) from 2014 to 2016 (72.7% men, mean age 65.6±13.8 years, age over 65 years in 72.7%).
In their study published in the journal BJBMS, the researchers defined neurological outcome by CPC scale I-V. Therapeutic measures were aimed to improve survival and neurological outcome of OHCA patients by optimal post-resuscitation care, including optimal circulation and oxygenation, early percutaneous coronary interventions (PCI) in acute coronary syndromes (ACS), therapeutic hypothermia.
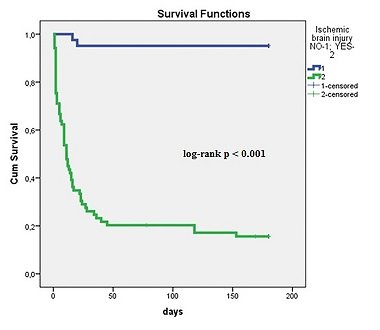
They observed good neurological outcome in 37.2%, severe ischemic brain injury in 62.7% of patients.
Severe ischemic brain injury was associated significantly with known pre-hospital data (older age, asystole as the cause of OHCA, longer resuscitations), but also with increased admission lactate, in-hospital complications (involuntary muscular contractions/seizures, heart failure, cardiogenic shock, acute kidney injury, mortality) and the need of inotropic and vasopressor support.
Good neurological outcome was associated with post-resuscitation early PCI and dual antiplatelet therapy in ACS and with better survival.
Reference:
Editor: Edna Skopljak
Leave a Reply